Why Are Cobra Insurance Premiums So High
COBRA insurance premiums are high because when you leave a job, you’re no longer part of an employer-sponsored health plan, which means you have to pay the full cost for the coverage. Usually, employers pay a significant portion of an employee’s healthcare premiums.
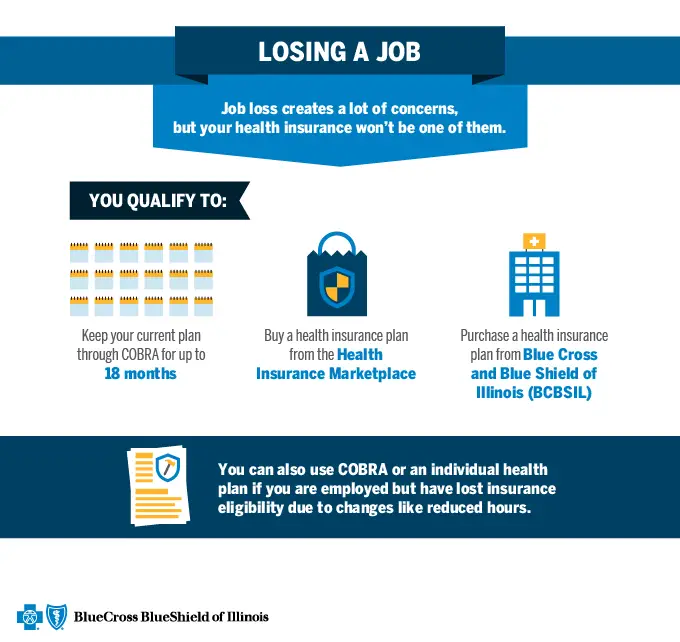
But even though COBRA premiums may be high, it’s still a good option for people who recently lost their jobs. That’s because COBRA allows you to keep your health insurance coverage for at least 18 months, which can be a big help if you have a pre-existing condition or need to see a specialist.
Which Companies Are Required To Provide Cobra7
Any company that had at least 20 employees on at least 50% of its business days during the previous year is required to provide COBRA coverage. Full-time and part-time employees are included in this qualifying count. In some states, those working for companies with less than 20 employees might qualify for “mini-COBRA” benefits thanks to state-specific laws that have been implemented since the initial Consolidated Omnibus Budget Reconciliation Act was passed in 1985. Check with your company’s benefits department or representative for more details.
However, churches and certain church-related organizations are not required to provide COBRA coverage. This also applies to plans sponsored by the federal government.
Changing From Family Plan To Single Plan
A single plan is simple enough to figure out with COBRA. It gets a bit more complicated if you need to switch from a family plan to a single plan. This can happen if you get divorced or turn 26 and are no longer eligible for coverage on your parents plan.
In instances like these, the HR officer will look up the rate for single coverage on the same health plan you are currently enrolled in. To calculate the COBRA cost, the HR officer will have to determine:
- What you would have been contributing to an individual plan. If you are a family member , your contribution would typically be higher than the employee . In some cases, dependents may be responsible for the entire amount if the employer does not contribute to family coverage.
- What the company would have been contributing toward that premium. If you are the employee , the amount should be clear-cut. If you are the dependent, the contribution can vary depending on the employer.
After adding these two figures together, you would add another 2% to calculate your total COBRA premium costs.
Don’t Miss: How Can I Change My Health Insurance
How Does Cobra Continuation Coverage Work
Under COBRA, former employees , spouses, former spouses of those employees, and dependents qualify for continued health coverage when it would typically end. In the U.S., any former employer with more than 20 full-time, active employees is required to offer COBRA continuation coverage by federal law.
As you might expect, the Covid-19 pandemic in 2020 has mandated a special enrollment period for COBRA benefits at healthcare.gov. This open enrollment period lasts only 60 days, but hopefully, this period will give you enough time to find better individual health insurance.
Most individuals can keep their COBRA coverage for 18 months or more. However, COBRA premiums are often more expensive than Medicaid, Medicare, or your states health insurance plans. Its meant to be a temporary interim solution, such as until your states next open enrollment period rolls around, rather than a a long-term health plan.
Make sure that you approve of your existing plan and its cost before you enroll for COBRA. Additionally, stopping your COBRA coverage early, just like any plan purchased through the health insurance marketplace, can result in penalties, so make sure to be aware of these in advance, too.
How Does Cobra Insurance Work If I Quit My Job

Whether you quit or lose your coverage in another way, the COBRA continuation coverage works the same.
Your employer will notify the health insurance company about the employment change within 30 days of your last day. Your health insurer will contact you with information about how you can sign up for COBRA and how much that coverage will cost you.
At that point, you have 60 days to sign up for COBRA insurance. You dont have to sign up immediately. You can delay sign up until the end of the 60-day period if you want.
Also Check: Can I Add My Mother To My Health Insurance
If I Drop Cobra Coverage During The Election Period Can I Get It Back On A Later Date
If you waive COBRA coverage, you can revoke the waiver later — as long as you’re still within the 60-day election period. The coverage is retroactive to when you became eligible for COBRA, as long as you pay the premiums retroactively.
You can also cancel COBRA coverage at any time — you’re not locked into an 18-month commitment when you sign up.
COBRA coverage ends when you:
- Reach the end of your coverage period
- Stop paying premiums
COBRA coverage also ends if the employer:
- Goes out of business
- Stops offering health insurance benefits to workers
If the employer changes health plans, you can switch to the new plan like everybody else, but you can’t keep the old plan in that case.
COBRA applies to private-sector companies with 20 or more employees as well as state and local governments. Some states also have “mini-COBRA” laws that apply to employers with fewer than 20 workers. See the section below for more information about mini-COBRA plans.
If you have a family health plan, not all family members have to enroll in COBRA. For instance, you can waive the option, but your spouse and kids could still elect COBRA, or vice versa.
Health Coverage For People With Disabilities
If you have a disability, you have three options for health coverage through the government.
-
Medicaid provides free or low-cost medical benefits to people with disabilities. Learn about eligibility and how to apply.
-
Medicare provides medical health insurance to people under 65 with certain disabilities and any age with end-stage renal disease . Learn about eligibility, how to apply and coverage.
-
Affordable Care Act Marketplace offers options to people who have a disability, dont qualify for disability benefits, and need health coverage. Learn about the .
Also Check: What Is The Most Affordable Health Insurance
If You Qualified For Cobra Premium Assistance
If you qualified for COBRA continuation coverage because you or a household member had a reduction in work hours or involuntarily lost a job, you may have qualified for help paying for your COBRA premiums .
COBRA premium assistance under the American Rescue Plan Act of 2021 was available April 1, 2021 through September 30, 2021. Since this help ended on September 30, you can enroll in a Marketplace plan with a Special Enrollment Period. To enroll, you can report a September 30 “loss of coverage” on your application. You cant qualify for a premium tax credit while youre enrolled in COBRA, so if you want to change to Marketplace coverage, make sure that your COBRA coverage ends on the last day before your Marketplace coverage can start. If you decide to keep COBRA without premium assistance, you can qualify for a Special Enrollment Period based on the end date of your COBRA coverage, which is usually 18 to 36 months after it started.
If you have questions about COBRA or COBRA premium assistance, visit the U.S. Department of Labor at DOL.gov or call 1-866-444-3272 to speak to a benefits advisor.
How Do You Qualify For Cobra
To be covered by COBRA:
Employers often meet the standard if they have more than 20 full-time employees. Churches and some other organizations, as well as health plans sponsored by the federal government, are exempt.
Being a qualified beneficiary means you were covered by the employer-sponsored plan at the time you lost coverage. Your spouse and other dependents may also be eligible.
Potential qualifying events include termination for any reason other than gross misconduct or reduced hours. For spouses and other dependents, there are a few other qualifying events, such as divorce or separation from the covered employee the death of the covered employee the covered employee becoming eligible for Medicare or loss of dependent-child status.
Don’t Miss: How To Get Health Insurance In Texas
How To Sign Up And Use Your Cobra Insurance
If you’ve lost your job or left for a new position, there may be a time when you dont have health insurance.
Consolidated Omnibus Budget Reconciliation Act insurance coverage was designed to provide people with a way to keep their existing health insurance for a period of time, until their new coverage takes effect.
Can I Continue My Cobra Coverage For A Longer Period
Yes, you can extend your COBRA continuation coverage under two circumstances under which you may be eligible for an extension. The first is when a qualified beneficiary becomes disabled and meets specific requirements, and then they are entitled to an 11-month extension on their maximum period of continuation coverage.
The second is if you experience another life event that qualifies you for an extension, such as-
- Divorce or legal separation
- Death of a covered employee
- If the qualified employee becomes eligible for a Medicare health care plan
- If you lose dependent child status under the program.
You May Like: Are You Required To Offer Health Insurance To Employees
What Do Qualified Individuals Need To Do To Obtain Coverage
Employees must elect COBRA coverage with their employee or COBRA administrator. Employers are responsible for notifying any subsidy-eligible participants,” said Rainey.
Generally, under the Department of Labor guidelines, employers have 60 days to notify you of your eligibility. Proactive employees have the green light to contact their employer to determine eligibility.
COBRA coverage doesn’t apply to co-pays or deductibles. If individuals decide to continue coverage beyond September 30, 2021, the premiums are no longer the employer’s responsibility.
Notices Required Of Qualified Beneficiaries
An employee or qualified beneficiary must notify the plan administrator of a qualifying event within 60 days after divorce or a child’s ceasing to be covered as a dependent under the plan’s rules. Also, a qualified beneficiary must notify the plan administrator within 60 days of those events when they occur during the initial 18 or 29-month period of coverage in order to qualify for an extension of the coverage period to 36 months.
If a second qualifying event is the death of the covered employee or the covered employee becoming entitled to Medicare benefits, a group health plan may require qualified beneficiaries to notify the plan administrator within 60 days of those events, as well. Ordinarily, the employer is responsible for notifying the plan administrator of an event that is the death of a covered employee or the covered employee becoming entitled to Medicare benefits. However, if the covered employee’s employment has been terminated, the employer may not be in a position to be aware of those events. If the plan does not require qualified beneficiaries to notify the plan within 60 days of a second qualifying event that is the death of the covered employee or the covered employee becoming entitled to Medicare benefits, a qualified beneficiary should provide that notice by the later of the last day of the 18-month period or the date that is 60 days after the date of the second event.
Don’t Miss: How To Apply For Medicaid Health Insurance
Make A Payment Within 45 Days
If you elect COBRA coverage, you have 45 days to pay the first month’s premium from the date you mailed in your election form. If you pay in full and on time, you’ll be retroactively covered. If you miss the payment, you could lose your ability to receive COBRA coverage entirely.
Coverage can last up to 18 months from the initial qualifying event , or longer in special circumstances such as retirement, disability, death, or divorce. If your monthly premiums aren’t paid in full and on time, the employer stops offering a group health plan, you become entitled to Medicare, you become insured by another plan, or you engage in fraud or otherwise shady conduct, your coverage could be terminated.
Editor’s note: A previous version of this article incorrectly stated that the total premium for COBRA cannot exceed 102% of the individual employee’s portion of the premium. The total premium cannot exceed 102% of the total cost of coverage, meaning it cannot be more than an employee’s portion, plus the employer’s portion, plus a 2% admin fee.
Cost Of Cobra Health Insurance
The term “group rate” may be incorrectly perceived as a discount offer, but in reality, it may turn out to be comparatively expensive. During the employment term, the employer often pays a significant portion of the actual health insurance premium , while the employee pays the remainder. After employment, the individual is required to pay the entire premium, and at times it may be topped up with an extra 2% toward administrative charges. Costs may not exceed 102% of the cost for the plan for employees who haven’t experienced a qualifying event.
Therefore, despite the group rates being available for the COBRA continued plan in the post-employment period, the cost to the ex-employee may increase significantly when compared to prior insurance costs. In essence, the cost remains the same but has to be borne completely by the individual with no contribution from the employer.
COBRA may still be less expensive than other individual health coverage plans. It is important to compare it to coverage the former employee might be eligible for under the Affordable Care Act, especially if they qualify for a subsidy. The employer’s human resources department can provide precise details of the cost.
Those who lost health insurance due to a job loss during the 2020 economic crisis, qualified for a “special enrollment” period on the federal exchanges, which gave them 60 days to sign up. That may have been a way to find a cheaper insurance option than COBRA.
Recommended Reading: Does Your Employer Pay For Health Insurance
Keep All Documents For Your Records
If you opt out of the COBRA option, you will receive a letter from the employer’s insurance company stating the dates that you were covered.
You should keep all records of coverage, in case you need them to prove you were covered during a period of time. For instance, the insurance company covering you might try to deny coverage by claiming that your policy had expired. Any records you keep can help you dispute the denial of coverage.
What Is Cobra Health Insurance
Large employers in the U.S., those with 50 or more full-time workers, are required to provide health insurance to their qualifying employees by paying a part of insurance premiums. If an employee becomes ineligible to receive an employer’s health insurance benefitswhich can happen for a variety of reasons the employer may stop paying its share of the employee’s insurance premiums. In that case, COBRA allows an employee and their dependents to retain the same insurance coverage for a limited period of time, provided they are willing to pay for it on their own.
Under COBRA, former employees, spouses, former spouses, and dependent children must be offered the option of continued health insurance coverage at group rates, which otherwise would be terminated. While these individuals are likely to pay more for health insurance coverage through COBRA than they did as employees , COBRA coverage might be less expensive than an individual insurance plan would be.
It’s important to note that COBRA is a health insurance coverage program and plans may cover costs toward prescription drugs, dental treatments, and vision care. It does not include life insurance and disability insurance.
As part of the American Rescue Plan Act of 2021, the federal government paid COBRA insurance premiums for individuals that lost their job as a result of the 2020 economic crisis from April 1 through Sept. 30, 2021.
Recommended Reading: When Health Insurance Open Enrollment
What Does Arp Cover
The ARP expands the original provisions of Families First Coronavirus Response Act by now including paid time off to obtain a COVID-19 vaccine as well as recovery time in response to the vaccination,” said Andrea Rainey, human resources business partner for The Strunk Insurance Group.
In addition, the government provides eligible employers tax credits for paid leave for employees for COVID-qualifying reasons,” said Rainey. The act creates a new COBRA premium subsidy from April 1 to September 30, 2021, for qualified individuals. The subsidy provides 100% of the premium for employees. In turn, employers and carriers will receive a tax credit to fund the subsidy.
Under normal circumstances, employees pay COBRA premiums, and these payments are traditionally more expensive than employer-provided insurance.
Can Continuation Coverage Be Canceled Early For Any Reason
A group health plan is allowed to terminate the continuation coverage before the maximum period for any of the reasons mentioned below-
- You haven’t paid the monthly payments on time.
- The employer or anyone who sponsored the plan no longer provides group health insurance coverage for its employees.
- A qualified beneficiary becomes eligible for another health care program.
- After selecting continuation coverage, a qualified beneficiary becomes eligible for Medicare benefits.
- If the qualified beneficiary commits any fraud or some other action that would lead to the termination of their coverage.
Recommended Reading: How Much Is Aetna Student Health Insurance
How Long Does The Cobra Coverage Last
The length of time you can keep COBRA coverage depends on your qualifying event . If your major medical coverage ends because your employment ends , or because your hours are reduced, you and your qualified dependents can keep coverage under the employers health insurance for up to 18 months by paying for the full cost of the coverage.
Note that a few states require employers to offer COBRA coverage for a longer time than federal laws do. Again, your state insurance commissioners office can tell you more about this.
