Our Drug & Alcohol Treatment Services Include
- Case management services: Every client is assigned a case manager upon his or her admission to our treatment program. The case manager walks the client through every step of the early recovery process, ultimately developing a long-term treatment plan that includes aftercare planning. Case managers also stay in communication with the loved ones of the client, providing updates on progress and informing of any future treatment plans.
- Intensive therapeutic care: We offer individual therapy sessions at least once every week, group therapy sessions on a daily basis and family therapy sessions as part of our comprehensive family-oriented treatment program.
- In-depth and thorough aftercare planning: Aftercare planning is crucial to the avoidance of relapse and the continuation of recovery. Our case managers help clients develop viable aftercare plans, ultimately making the transition from medical detox to inpatient rehab as seamless as possible.
Does First Health Cover Therapy
Yes, First Health covers therapy services for its members. However, because First Health is such a large health insurance company, they offer many plans across the country and the mental health benefits will vary depending on which plan you have.
For individuals who have First Health, seeing a therapist who is in-network with First Health is typically the most cost-effective option, as youll pay less out-of-pocket.
First Health Networkinsurance For Addiction Recovery
First Health Network is one of the largest national PPO networks available in the United States. PPO networks refer to a type of managed care health insurance plan that provides maximum benefits if you visit an in-network physician or provider, while at the same time provides some coverage for out-of-network providers. In-network essentially means that any specific healthcare provider is covered in full by a specific insurance plan. For example, the services that Immersion Recovery Center offers are typically covered in full by First Health Network Insurance. Behavioral health services like medical detox and residential addiction treatment are now considered essential components of comprehensive healthcare. Any major insurance providers that cover standard healthcare services also cover addiction-related services. At Immersion Recovery Center we understand that figuring out how to cover the cost of a multi-phased continuum of care can seem overwhelming to our clients and their loved ones, especially if they are unaware of the numerous financial resources that are available to them. We gladly walk you through every step of the admissions process from travel plans to insurance benefit checks.
Recommended Reading: What Health Insurance Does Starbucks Offer
First Health Insurance Company
First Health Insurance Company is a subsidiary of Coventry Health Care and is based in San Diego, California. They offer a nationwide PPO network to serve the needs of clients who manage employee health benefits plans. The company currently serves over 3.5 million people throughout the United States. First Health prides itself on superior access to healthcare providers across the country at a reasonable rate.
Compare rates from First Health to other health insurance providers in your area. Click here and enter your zip code for a list of rates from local health insurance providers.
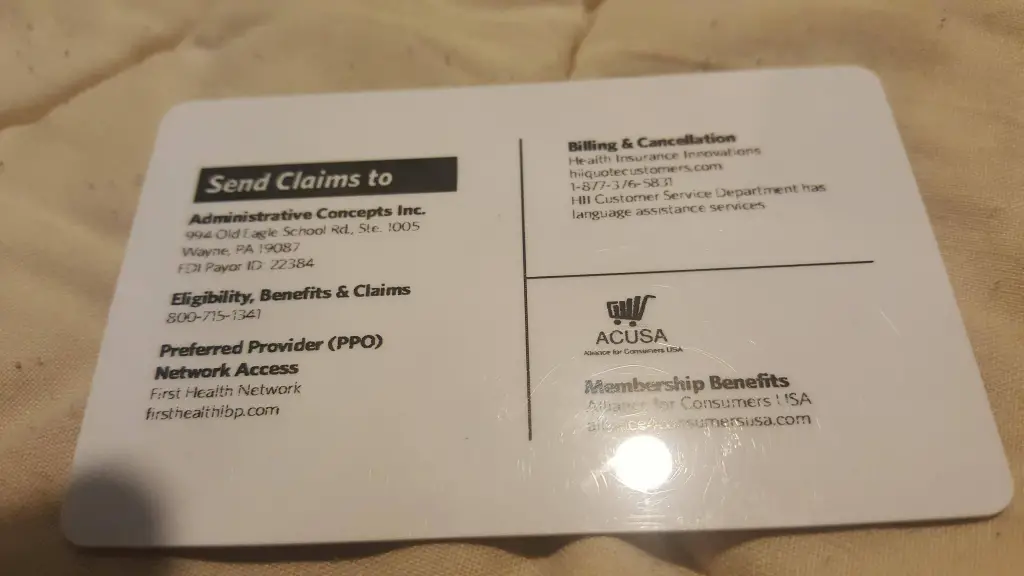
First Health Insurance Claims
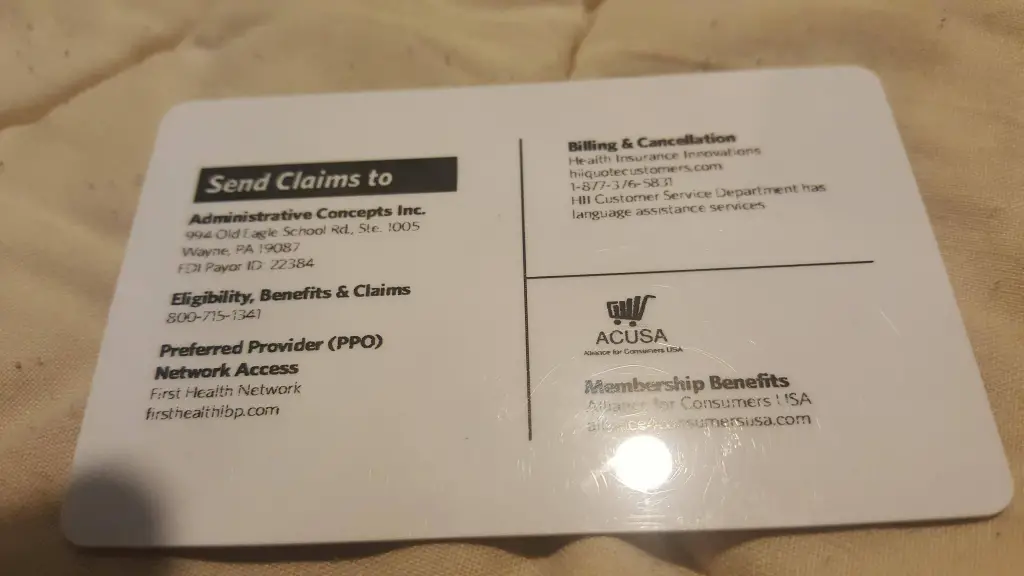
You will never have to fill out any claims forms with First Health, nor will you have to contact the company yourself when faced with an illness or injury. Instead, if you need to see a specialist, ask your primary doctor to refer you to one within the First Health Network. You do not have to do anything else.
If you are admitted to a hospital in an emergency situation, you should have the hospital contact the First Health review organization that is listed on your insurance card within 24 hours of being admitted. Once again, you do not have to do anything else, allowing you to focus on your health and healing.
Get health insurance quotes from companies like First Health in your local area. Simply click here and enter your zip code for a free list of health insurance quotes.
Recommended Reading: How Much Does Starbucks Health Insurance Cost
Does First Health Insurance Cover Inpatient Mental Health Treatment Facilities
Understanding your First Health mental health coverage is vital to a successful recovery for most people. According to research, many people who have a substance use disorder also have a mental health disorder.6 Treating these conditions simultaneously is best for a successful recovery.5 Common mental illnesses that co-occur with substance use disorder include: 6
- Anxiety, including panic disorders
- Psychotic illness
- Borderline personality disorder
People who have co-occurring disorders may become addicted to any substance, including opioid painkillers, cocaine, heroin, alcohol, meth, and benzos. Research indicates that people who are in treatment for abusing prescription pain medications are likely to have symptoms of anxiety and depression.6
If you think you might have co-occurring conditions, its best to seek treatment with a provider who manages both conditions. You can request a First Health mental health provider list and contact the facility for more information. You dont need to worry about your First Health benefits covering you for both disorders. Under the Affordable Care Act, insurance carriers are required to provide coverage for mental health disorders and substance addiction treatment.7
Does First Health Cover Couples Therapy
No, First Health does not cover couples therapy. This is partially because its difficult to provide that diagnosis for the mental health condition as required by many insurance companies for reimbursement.
However, if youre still interested in working with a couples therapist, there are ways to access couples therapy on a budget.
Also Check: Starbucks Employee Health Insurance
About First Health Coverage For Detoxification
For many, detox is a medically necessary first step to recovery. We strongly advise clients who need to detox to do so safely under the clinical supervision of a treatment center. Although the Mental Health Parity and Addiction Equity Act of 2008 makes coverage for substance abuse and mental health a federal law, not all PPOs cover detox. If your First Health PPO insurance does cover detox, you might have to pay a deductible first, meaning your policy will only cover its portion after you pay for a certain amount in out-of-pocket costs. Its a good idea to check with your insurance company to see if youve already met your deductible or how close you might be to reaching it.
First Health Network Advantages
When you use a provider within the First Health Network you not only save yourself money, you gain several other advantages. Aside from only paying a co-pay, you also never have to fill out a claims form. All claims are filed for you. Additionally, since First Health receives contracted rates from providers, services cost less and the company can offer lower co-pays.
Unlike most health insurance companies, most plans within the First Health PPO network do not require you to select a primary care physician. The company does recommend having one however, because this doctor can be the keeper of all of your medical information, which helps when you have medical questions or need support in dealing with an illness or other medical issue.
Read Also: Starbucks Insurance Enrollment
First Health Insurance Ppo: Customer Service
First Health Ppo Reviews Customer service is an integral part of insurance service and when it comes to health insurance its importance cannot be emphasized enough. Most customers that have been in contact with the customer service from First Health can easily testify and agree with us that there is not service that comes closer in America if not the world.
The professionally trained staff is friendly and also the fact that the company has a huge staff complement means that great service is just a request away. We can only hope that the company continuously progress and maintain their customer service.
Emergency Care And Surprise Balance Billing
The Affordable Care Act requires health plans to cover out-of-network emergency services with the same cost-sharing they would use if the provider had been in-network. This means your applicable deductible, copays, and coinsurance for the emergency care will be the same as they would have been if you’d received the emergency care in-network.
But prior to 2022, federal rules did not prevent out-of-network hospitals and emergency medical providers from balance billing patients for emergency care. This is known as “surprise balance billing,” because the emergency nature of the medical treatment prevented the patient from actively determining beforehand whether all of the participants in their care were in-network. Surprise balance billing also refers to situations in which a patient goes to an in-network hospital but unknowingly receives care from an out-of-network provider while at the facility.
Numerous states had stepped in with laws and regulations to address surprise balance billing, opting for various provisions that hold the patient harmless in situations like this, but these laws didn’t apply in all states and didn’t apply to self-insured health plans, which are regulated at the federal level instead.
Fortunately, the federal No Surprises Act took effect in 2022, prohibiting surprise balance billing in most circumstances .
You May Like: Starbucks Part Time Health Insurance
First Health Insurance Review
If you are out of work, yet wish to be employed in a few several weeks with a company that provides team insurance, than probably temporary elderly insurance plan for seniors security is for you.
Also some companies need a new worker to work for three to six several weeks before they are qualified for wellness benefits. Short term could offer the temporary security you need. Next, decide if primary health-care security or comprehensive wellness good care protection will much better meet your needs.
What Our Clients Are Saying
-
I love these products! For the past 6 months Ive made HFN products part of my routine and I feel healthier and happier. Thanks for all the incredible insights as well!
– First
I love these products! For the past 6 months Ive made HFN products part of my routine and I feel healthier and happier. Thanks for all the incredible insights as well!
– Second
I love these products! For the past 6 months Ive made HFN products part of my routine and I feel healthier and happier. Thanks for all the incredible insights as well!
– Third
-
I love these products! For the past 6 months Ive made HFN products part of my routine and I feel healthier and happier. Thanks for all the incredible insights as well!
– Fourth
I love these products! For the past 6 months Ive made HFN products part of my routine and I feel healthier and happier. Thanks for all the incredible insights as well!
– Fifth
Read Also: Kroger Health Insurance Part-time
Comprehensive Health Care Coverage
This first health insurance includes precautionary good proper care, Drs visits, medications, along with hospitalizations and out-patient surgery treatment therapy.
Extensive wellness excellent care safety has a higher per month top high quality, and it generally has a low co-pay at the time of a Drs consultation. This first health insurance may be the much better choice appropriate for those who have reoccurring healthcare care costs.
What Types Of Mental Health Conditions Does First Health Cover
First Health insurance covers services for many mental health conditions. To reimburse therapists or clients, First Health requires that the client receive a diagnosis from their therapist. This diagnosis guides treatment and the insurance coverage.
Examples of eligible mental health conditions include:
There are many more types of therapies and often, therapists blend modalities into their own approaches, all of which are covered by First Health. First Health requires its providers to have the appropriate credentials and trusts that these providers maintain high professional standards.
Don’t Miss: How To Get Insurance Between Jobs
Begin Your Personal Journey Of Addiction Recovery
We understand how overwhelming the financial components of a comprehensive recovery program can seem to our clients and their loved ones. For this reason, we work closely alongside national health insurance providers like First Health Network in order to provide the highest level of clinical care available to all those who require medical detox and inpatient treatment services. If you or someone you love has been suffering at the hands of a substance abuse disorder of any severity, Princeton Detox & Recovery Center is available to help. Give us a call and our Treatment Advisors will conduct a brief pre-assessment over the phone, which helps us determine which level of clinical care is the most appropriate for each unique case. Once the assessment is complete and it is determined that our program of recovery is a good fit, we conduct a brief insurance benefit check and set up a date and time for intake.
First Health Pp Review
The first thing you might need to know just how big, First Health Ppo is. There seems to be a huge misconception about the company and we are about to clear it. first Health Ppo is affiliated with over 5900 hospitals and if you think that number is huge then the number of staff will shock you to the core. First Health has a staff complement of up to eight hundred thousand That is nearly a million workers.
This makes the company a huge player in the health insurance market. The main reason why a company grows that huge has to be due to a lot of positive for the customers. Lets look at some of the pros that we managed to pick out from the reviews we looked at.
Read Also: Evolve Health Insurance Company
Programs Covered By First Health Network
- Medical detox: Medically monitored detox is the first stage of every successful long-term recovery process. During medical detox clients are closely monitored by a team of medical professionals, and they undergo a safe and pain-free withdrawal in a secure, private and homestyle setting.
- Addiction treatment services: At Princeton Detox & Recovery Center we offer a wide range of addiction treatment services, all geared towards helping our clients prevent relapse and maintain long-term and fulfilled recovery.
- Comprehensive aftercare planning: No treatment program is complete without in-depth aftercare planning. In most cases, this will include a transition from medical detox to inpatient treatment and a wide variety of additional, recovery-related services.
- Case management services: Upon admission to our medical detox or inpatient treatment facility, clients are assigned a case manager who will walk them through every single stage of the recovery process.
- In-depth clinical and medical assessments: As soon as a client is admitted to our treatment center, he or she will undergo an in-depth clinical and medical assessment. During this assessment, our clinical team asks the client a specifically designed set of questions that illuminates personal history with substance abuse, underlying mental health disorders and all other contributing factors.
- Therapeutic services: We offer individual, group and family therapy services to each of our clients.
Policy Coverage For Substance Abuse With First Health
As we mentioned, the level of coverage offered by your insurance company depends on your current policy. Having said that, there is a good chance your First Health plan will cover at least a portion of the costs for your time spent at a treatment center whether its detox, residential rehab, or an outpatient treatment.
This usually includes hospitalization relating to substance abuse, clinical assessments, diagnoses, drug tests, and any other lab work you may need as part of your treatment. Additionally, rehabilitation services will likely include coverage for a co-occurring mental health disorder, medication-assisted treatment, family support therapy, and recovery maintenance, such as continuing care programs or follow-up counseling.
Don’t Miss: Starbucks Insurance Plan
How Much Does Therapy Cost With My First Health Plan
When you see a therapist within the First Health network, you may have a copayment of around $50/session, though the cost for therapy depends on which plan you have. There are many plans offered through First Health, which vary based on family size and geography, and result in a different copayment. First Health does not provide coverage for out-of-network therapists.
First Health Ppo Reviews: Accessibility
First Health Ppo Reviews The first thing we have to compliment about the company has to be the companys extensive accessibility. It is rare to find a health insurance service that is available in nearly every place in the United States, well was rare because First Health Ppo has managed to easily do that, The First Health Ppo insurance gives you access to over give thousand medical facilities in the United States This means chances are the nearest hospital near you is affiliated with First Health insurance.
This is one of the aspects that service users cannot stop bragging about in their reviews. The company has promised to continuously drive and expand their service and we hope they stick to their word.
Recommended Reading: Does Starbucks Have Health Insurance
What Is Fair And Reasonable Sharing
Fair and Reasonable Sharing is our model that reimburses Providers at a fair price when compared to services performed. We lower Member costs for most services by using a percentage above Medicare allowable. In most cases, the Provider will accept this initial sharing amount as payment-in-full. However, if a Provider insists on charging our Members more than the initial sharing amount and sends them another bill, weve got their back! OneShare Health’s trained team of Coordinators will contact the Members Provider and work toward a resolution that doesnt leave them holding the bag.
Available Individual And Family Insurance Plans
Health good care applications generally fall into two groups, indemnity or managed-care applications. They vary in respect to how costs are paid, ability to select healthcare companies and out-of wallet expenses.
Usually, youll have a broader option of healthcare companies with indemnity health-care applications and less out-of -pocket costs and less paperwork with a managed-care first health insurance protection strategy.
Recommended Reading: Does Starbucks Provide Health Insurance
