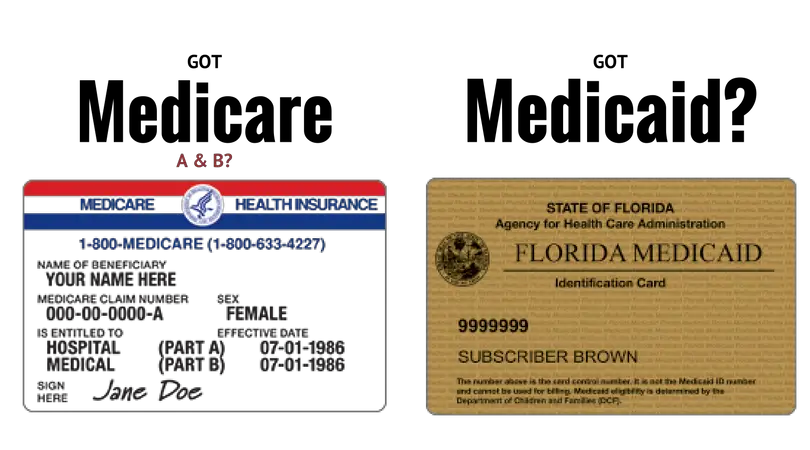
Who Qualifies For Both Medicare And Medicaid
A: In many cases, yes. Some people do qualify for both Medicare and Medicaid, and in those instances, most of the enrollees health care costs are covered. People who are eligible for Medicaid and Medicare are known as dual eligible. About 20 percent of Medicare beneficiaries are also eligible for Medicaid.
Unitedhealthcare Dual Complete Plans
Plans are insured through UnitedHealthcare Insurance Company or one of its affiliated companies, a Medicare Advantage organization with a Medicare contract and a contract with the State Medicaid Program. Enrollment in the plan depends on the plans contract renewal with Medicare. This plan is available to anyone who has both Medical Assistance from the State and Medicare. This information is not a complete description of benefits. Call TTY 711 for more information. Limitations, co-payments, and restrictions may apply. Benefits, premiums and/or co-payments/co-insurance may change on January 1 of each year.
How Medicaid Eligibility Is Determined
Income eligibility is determined by your modified adjusted gross income , which is your taxable income, plus certain deductions. Those deductions include non-taxable Social Security benefits, individual retirement contributions and tax-exempt interest. For most people, MAGI is identical or very close to your adjusted taxable income, which you can find on your tax return. Specific income requirements in dollars rise alongside the size of your household.
Our guide focuses on each stateâs major programs for adults. Most are only available to state residents, U.S. citizens, permanent residents or legal immigrants .
Looking for insurance for a child? Check out our guide to the Children’s Health Insurance Program .
Recommended Reading: How To Sign Up For Obama Care Health Insurance
How Medicaid Works With Other Health Coverage
Sponsored by HMS
According to CMS data, more than 72 million Americans rely on Medicaid and the Childrens Health Insurance Program for health insurance, making Medicaid the largest source of health coverage in the nation. Since the Affordable Care Act of 2010 gave states the option to expand Medicaid to nearly all low-income Americans, Medicaid enrollment has surged, with Washington, D.C., and 36 states opting to expand coverage to date.
While the extent of coverage varies by state, the list of benefits required by federal law make Medicaid coverage quite comprehensive. There are, however, instances in which an individual might have Medicaid in addition to one or more third-party payers. These include, but are not limited to:
- Other government-subsidized coverage. An individual is entitled to additional benefits under Medicare, CHIP or another public health insurance program.
- Commercial health coverage. An individual might be enrolled in an employer-issued or private health plan while also qualifying for Medicaid.
- Managed care contracts. The state agency has contracted a managed care organization to coordinate patient care.
Coordinating Medicaid and Medicare BenefitsFor individuals who are eligible for both Medicare and Medicaid , Medicare is the primary payer for services covered by both programs.
What To Do If You Don’t Qualify For Medicaid

If you don’t qualify for Medicaid, you can possibly get subsidized health care through the Obamacare marketplaces during a special enrollment or open enrollment period. Americans who make between 100% and 400% of the FPL qualify for a premium tax credit that can significantly lower the cost of a plan.
Federal open enrollment for 2019 health care plans ended on Dec. 15, 2018, though some state exchanges are open longer and Nevada sells health insurance all year round. Learn 2020 open enrollments dates by state. Healthcare.gov, the federal exchange, usually opens from November 1 to December 15 each year.
If you can’t find affordable health care on your marketplace during open enrollment, you have a few back-up options.
These include:
Short-term health insurance: Originally designed to prevent short-term health insurance gaps, these plans are cheaper, but much less comprehensive than traditional coverage. They don’t have to cover Obamacare’s ten essential benefits or pre-existing conditions. Following changes by the Trump administration, short-term health plans can last from three months to potentially three years.
Limited benefit plans: These plans cover a very small portion of the costs associated with certain “medical events”, like a doctor’s visit or ambulance ride. Both the number of events and dollar amounts covered are capped.
Read Also: What Is The Best Supplemental Health Insurance For Medicare
Q What Documents Will I Need To Provide When I Apply
A. You will need to provide verification of your income. You do not need to provide proof of your assets or resources or come into our offices to be interviewed unless you are applying for one of the Long Term Care Medicaid programs .
If you are pregnant, you will need to provide proof that you are pregnant. If you are not a U.S. citizen, you will need to provide proof of your alien status. For example, you can provide a copy of your green card.
If you apply online using ASSIST, a web page at the end of the application will tell you exactly what documents must be sent by mail to support the application you are submitting, and the appropriate mailing address.
How Does The Irs Know If You Have Health Insurance
The health insurance coverage you have during the year will be reported to the federal government when you file your annual taxes. Health insurers, employers that sponsor health plans and agencies that administer government health plans will file annual reports to the IRS about who is covered under their plans.
You May Like: Can You Put Boyfriend On Health Insurance
Service Changes Due To Covid
You may not need to renew your health card at this time. Most expired health cards remain valid until further notice.
Health care providers have the tools to validate your card each time you visit. You can check whether your card is valid by calling ServiceOntario at 1-866-532-3161 . If it is no longer valid, you will need to update your health card registration by visiting a ServiceOntario centre. Learn more about the OHIP eligibility requirements.
As of March 19, 2020 we are waiving the three-month waiting period for OHIP coverage. If you do not meet the criteria for OHIP coverage and are uninsured, the province will fund the cost of COVID-19 services.
What Happens If Someone Cant Afford Healthcare
If you dont have health insurance for 3-month period or more, you may have to pay penalties to the government called individual shared responsibility payment, which is the ACA penalty. You may qualify for an exemption. Keep in mind that inability to pay doesnt automatically mean that you will avoid penalties.
Recommended Reading: Can You Get Health Insurance Immediately
Minimum Essential Coverage And Tax Penalties
Q. Who is required to have Minimum Essential Coverage ? A. All U.S. citizens living in the United States are required to have health coverage or insurance that meets the Affordable Care Act’s definition of Minimum Essential Coverage . Otherwise, you may have to pay a tax penalty called the “shared responsibility provision.” Citizens required to have MEC also include:
- Children –
- Each child in a family must have MEC or the adult claiming the child as a dependent may have to pay the penalty.
- Senior Citizens –
- Aside from Medicaid, Medicare Parts A and C qualify as MEC.
- Foreign Nationals and Resident Aliens –
- You are required to have MEC if you have been in the U.S. long enough during a calendar year to qualify as a resident alien for tax purposes. If you have to file a tax return, but have not been in the U.S. long enough to be considered a resident alien, you are not required to have MEC.
- U.S. Citizens Living Abroad –
- You are required to have MEC unless you have not been physically present in the United States for at least 330 full days within a 12-month period or if you are considered a bona fide resident of a foreign country for an entire taxable year.
If you don’t file a tax return, you can also apply for the exemption using forms available at healthcare.gov .
Will My Medicaid Cancel If I Get Insurance
Medicaid is a low-cost health care insurance sponsored by the federal government and administered by the states. As long as you meet the requirements for Medicaid, the government will not cancel your coverage, even if you have private insurance. Because no health insurance covers everything, having supplemental coverage to expand your Medicaid is encouraged if you can get it.
Don’t Miss: How To Get Health Insurance For My Family
Medicaid Is Jointly Financed By States And The Federal Government
Medicaid is financed jointly by the federal government and states. The federal government matches state Medicaid spending. The federal match rate varies by state based on a federal formula and ranges from a minimum of 50% to nearly 75% in the poorest state. Under the ACA, the federal match rate for adults newly eligible was 100% for 2014-2016, phasing down gradually to 90% in 2020 and thereafter . The federal matching structure provides states with resources for coverage of their low-income residents and also permits state Medicaid programs to respond to demographic and economic shifts, changing coverage needs, technological innovations, public health emergencies such as the opioid addiction crisis, and disasters and other events beyond states control. The guaranteed availability of federal Medicaid matching funds eases budgetary pressures on states during recessionary periods when enrollment rises. Federal matching rates do not automatically adjust to economic shifts but Congress has twice raised them temporarily during downturns to strengthen support for states.
Total federal and state Medicaid spending was $577 billion in FY 2017. Medicaid is the third-largest domestic program in the federal budget, after Social Security and Medicare, accounting for 9.5% of federal spending in FY 2017. In 2017, Medicaid was the second-largest item in state budgets, after elementary and secondary education .
Figure 8: Medicaid is a budget item and a revenue item in state budgets.
What Makes Health Care So Expensive

The price of medical care is the single biggest factor behind U.S. healthcare costs, accounting for 90% of spending. These expenditures reflect the cost of caring for those with chronic or long-term medical conditions, an aging population and the increased cost of new medicines, procedures and technologies.
Don’t Miss: How To Check If You Still Have Health Insurance
Two Categories Of Medicaid Eligibility
Before the Affordable Care Act, Medicaid eligibility was based on how much money you earned and how much you owned, e.g., your income, your assets, and your net worth. After the law was enacted, however, eligibility was split into two distinct groups.
Some people continued to qualify for Medicaid the old fashioned way, while others qualify based on their modified adjusted gross income .
Q If I Have Private Health Insurance Can I Be Eligible For Medicaid
A. It depends. If your income is low, and you have minor children, you and your children can have private health insurance and still be eligible for Medicaid. Certain Medicaid qualifying programs require that you not have any other health insurance in order for you to get Medicaid. If you have both private health insurance and Medicaid, you should show both your Medicaid card and your private health insurance card to your medical provider each time you receive services.
Also Check: Can I Get Health Insurance In Another State
Do Medicaid Patients Get Treated Differently
A study of hospitals in Florida has found some evidence that, compared to other patients in the same hospital, uninsured and Medicaid patients are treated by lower-quality physicians. This difference may indicate that physicians alter their treatment practices based on the generosity of patients insurers.
Funeral And Burial Funds
The government allows some dignity when it comes to death and dying. Funds used to pre-arrange a funeral or memorial are excluded from your Medicaid assets. This includes pre-purchased burial plots, not only for you but for your immediate family.
If no preparations are made in advance, a bank account up to $1,500 can be reserved for funeral expenses and not be counted towards your Medicaid qualifying assets.
You May Like: Is It Required For Employers To Offer Health Insurance
Q Who Qualifies For Medicaid
A. Citizenship and Residency – To obtain full Medicaid benefits in Delaware, you must be a Delaware resident and either a U.S. citizen or a legally residing noncitizen. Full coverage for noncitizens which include DACA recipients is dependent on the availability of state funding. However, noncitizens can qualify for coverage for emergencies and labor & delivery services if income requirements are met.
Income Level – Qualifying for Medicaid is also based on need. Household income must be under certain limits as defined by the Federal Poverty Level and is based on family size. For Long Term Care programs, financial resources must also be under a certain amount. There are also specific programs for individuals who meet certain medical or disability tests, or who qualify due to age or pregnancy. To find out more about different Medicaid and other medical assistance programs, visit DMMA Programs & Services.
Medicaid Covers 1 In 5 Americans And Serves Diverse Populations
Medicaid provides health and long-term care for millions of Americas poorest and most vulnerable people, acting as a high risk pool for the private insurance market. In FY 2017, Medicaid covered over 75 million low-income Americans. As of February 2019, 37 states have adopted the Medicaid expansion. Data as of FY 2017 show that 12.6 million were newly eligible in the expansion group. Children account for more than four in ten of all Medicaid enrollees, and the elderly and people with disabilities account for about one in four enrollees.
Medicaid plays an especially critical role for certain populations covering: nearly half of all births in the typical state 83% of poor children 48% of children with special health care needs and 45% of nonelderly adults with disabilities and more than six in ten nursing home residents. States can opt to provide Medicaid for children with significant disabilities in higher-income families to fill gaps in private health insurance and limit out-of-pocket financial burden. Medicaid also assists nearly 1 in 5 Medicare beneficiaries with their Medicare premiums and cost-sharing and provides many of them with benefits not covered by Medicare, especially long-term care .
Figure 4: Medicaid plays a key role for selected populations.
Read Also: Is It Required By Law To Have Health Insurance
How Does Hipp Work
HIPP will pay your health plan’s premium if it costs less than covering your family through Medicaid. The program allows you to keep the insurance you get through your job and keep your Medicaid benefits.
- The family member who has Medicaid and the family member who can get employer-sponsored health insurance can be any age.
- The employer-sponsored health plan must be able to cover the family member who has Medicaid.
When you join, the state will pay you back for your premiums, and you’ll be able to choose from more health care providers than with Medicaid alone.
Unitedhealthcare Connected Benefit Disclaimer
This is not a complete list. The benefit information is a brief summary, not a complete description of benefits. For more information contact the plan or read the Member Handbook. Limitations, copays and restrictions may apply. For more information, call UnitedHealthcare Connected Member Services or read the UnitedHealthcare Connected Member Handbook. Benefits and/or copayments may change on January 1 of each year.
Also Check: Does Health Insurance Cover Pre Existing Conditions
Policy Basics: Introduction To Medicaid
In 2018, Medicaid provided health coverage for 97 million low-income Americans.
In 2018, Medicaid provided health coverage for 97 million low-income Americans over the course of the year. In any given month, Medicaid served 32 million children, 28 million adults , 6 million seniors, and 9 million people with disabilities, according to Congressional Budget Office estimates.
Children account for more than two-fifths of Medicaid enrollees but only one-fifth of Medicaid spending. Only one-fifth of Medicaid enrollees are seniors or people with disabilities, but because they need more health care services, they account for nearly half of Medicaid spending.
Medicaid is sometimes confused with Medicare, the federally administered, federally funded health insurance program for people over 65 and some people with disabilities. And there is overlap between the two programs: nearly 10 million low-income seniors and people with disabilities so-called dual eligibles are enrolled in both Medicare and Medicaid.
Unitedhealthcare Senior Care Options Plan
UnitedHealthcare SCO is a Coordinated Care plan with a Medicare contract and a contract with the Commonwealth of Massachusetts Medicaid program. Enrollment in the plan depends on the plans contract renewal with Medicare. This plan is a voluntary program that is available to anyone 65 and older who qualifies for MassHealth Standard and Original Medicare. If you have MassHealth Standard, but you do not qualify for Original Medicare, you may still be eligible to enroll in our MassHealth Senior Care Option plan and receive all of your MassHealth benefits through our SCO program.
You May Like: Can I Buy Dental Insurance Without Health Insurance
Q How Long Will My Medicaid Benefits Remain Active
A. Medicaid is based on month to month eligibility. However, your benefits are redetermined on a yearly basis by DMMA to confirm whether you still remain eligible for the program you are receiving. Certain Medicaid programs require you to report changes in your situation within 10 days of the change. One example of a change that must be reported is new employment.
