How K Health Can Help
Did you know you can get affordable primary care with the K Health app?
to check your symptoms, explore conditions and treatments, and, if needed, text with a doctor in minutes. K Healths AI-powered app is HIPAA compliant and based on 20 years of clinical data.
K Health articles are all written and reviewed by MDs, PhDs, NPs, or PharmDs and are for informational purposes only. This information does not constitute and should not be relied on for professional medical advice. Always talk to your doctor about the risks and benefits of any treatment.
K Health has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references.
Small Steps To Ensure That You Do Not Lapse Your Health Insurance Plan Next Time
Update your email id and phone number accurately with the insurer and update the same in case of a change, so that you do not miss renewal calls, emails, etc.
You can also create a standing instruction on your account, credit card, etc. so that the renewal gets automatically processed even if you are busy or out-of-the-country or unable to pay within the grace period. This way, you can never miss your renewal lifelong!
With the technology at our side, there is no excuse for missing renewal payment. It can be done seamlessly through net banking, phone banking, app banking, etc. and just with the click of a button.
Featured Articles
Notices Related To Cobra Continuation Coverage
When you or your employer notifies the Plan that your health care coverage has ended due to a Qualifying event, then the Trust Fund Office will give you and/or your covered Dependents notice of the date on which your coverage ends and the information and forms needed to elect COBRA Continuation Coverage. Failure to notify the Plan in a timely fashion may jeopardize an individuals rights to COBRA coverage. Under the law, you and/or your covered Dependents will then have only 60 days from the date of receipt of that notice, to elect COBRA Continuation Coverage.
| NOTE: If you and/or any of your covered Dependents do not choose COBRA coverage within 60 days after receiving notice, you and/or they will have no group health coverage from this Plan after the date coverage ends. |
Don’t Miss: Starbucks Pet Insurance
Entering Into An Agreement With The Commission To Participate In The Ei Program
Self-employed persons must have entered into a formal agreement with the Canada Employment Insurance Commission in order to participate in the EI program. At least 12 months must elapse from the time the agreement is entered into before a self-employed participant would be eligible for EI special benefits. This agreement triggers the payment of EI premiumsFootnote 2.
What Is Term Plan
Amongst the myriad of insurance options out on the market, a term insurance policy is probably one of the most affordable ways to secure your loved ones. When you choose term insurance plans, your nominee becomes eligible to receive a death benefit that could help them lead a stable lifestyle in case anything uncertain were to happen to the life assured.
Take for example that a policyholder has a term life insurance cover of 1 crore for a policy term, which lasts approximately ten years. If the life assured were to die in these ten years, the insurance company will give out the entire 1 crore sum to the nominee or beneficiary of that policy. Let us say that the policyholder survives the term of the policy. If a pure term plan was selected, the plan will then expire with no benefit paid out to either the policyholder or her/his nominees.
Read Also: Starbucks Insurance Plan
Aging Out Of Your Parents Plan
Under the ACA, you can stay on your parents healthcare plan until you turn 26, regardless of whether you live with them. If you graduate from college and move to a different state, you can still have access to your parents health insurance . Even if you get married or have your own child before the age of 26, you may still be eligible for the healthcare benefits that your parents receive.
Depending on the kind of healthcare coverage your parents have, you may lose coverage immediately on the day you turn 26. Some plans allow young adults to remain on their parents plans until the end of the month following their 26th birthday. Others let them stay on their parents plans until the end of the tax year.
Because different healthcare plans have different rules, its best to find out when coverage will end for your parents specific plan. That way, youll know when youll need to purchase health insurance. If you lose health insurance following your 26th birthday and youre uninsured for more than three months in a row, you may have to pay a fine.
How To Renew/revive Lapsed Health Insurance Policy
However, if your health plan has not been renewed and has lapsed beyond the grace period, all you need to do is buy a fresh plan. Since the same cannot be renewed now, you can either continue the same plan with your earlier insurance company by simply paying the premium and undergoing a pre-medical check-up, if the lapse is more than 6 months or compare and then buy a fresh health insurance plan for yourself which suits your needs the best.
Also Check: Starbucks Insurance Benefits
Federal Cobra Subsidies In The American Rescue Plan
The American Rescue Plan, enacted in March 2021, is a sweeping COVID relief measure. Among many other things, it provides the third round of stimulus checks to most Americans, extends the additional federal unemployment compensation that began soon after the pandemic started, and makes health insurance more affordable for millions of people.
One of the health insurance provisions is a temporary federal subsidy that covers 100% of the cost of COBRA coverage from April 1, 2021 through September 30, 2021, for people who involuntarily lost their jobs or had their hours reduced below the level that makes health insurance available. This subsidy is outlined in Section 9501 of the American Rescue Plan.
The federal COBRA subsidy is available to people already enrolled in COBRA, and to people who newly enroll in COBRA during the April – September window. But again, it’s only available if you involuntarily lost your job or had your hours reduced if you left your job voluntarily or opted to transition to part-time work, you would not be eligible for the COBRA subsidy.
Now let’s take a look at how COBRA rules normally work, and how they’re expected to once again work after the COVID pandemic subsides:
Early Termination Of Cobra Continuation Coverage
Once COBRA Continuation Coverage has been elected, it may be cut short on the occurrence of any of the following events:
Also Check: Starbucks Health Insurance Eligibility
How To Enroll In A Healthcare Plan
When youre ready to purchase your own health insurance, you have several options. You can speak to someone in the human resources department about enrolling in a healthcare plan provided by your employer. You could also ask whether you qualify for COBRA coverage under your parents plan.
Through the Consolidated Omnibus Budget Reconciliation Act , you may be able to retain coverage under your parents healthcare plan for up to 36 months after turning 26. To be eligible for COBRA coverage, youll have to submit a written request to your parents boss. If your parent works for a company with fewer than 21 employees, your state may offer temporary health insurance that functions like COBRA coverage.
A third option is to sign up for a plan through the Health Insurance Marketplace. Lower-income individuals may qualify for the premium tax credit that reduces their tax liability. But government subsidies may no longer be available if key components of the ACA go up in flames. If you think you may qualify for Medicaid, thats another route you may need to explore.
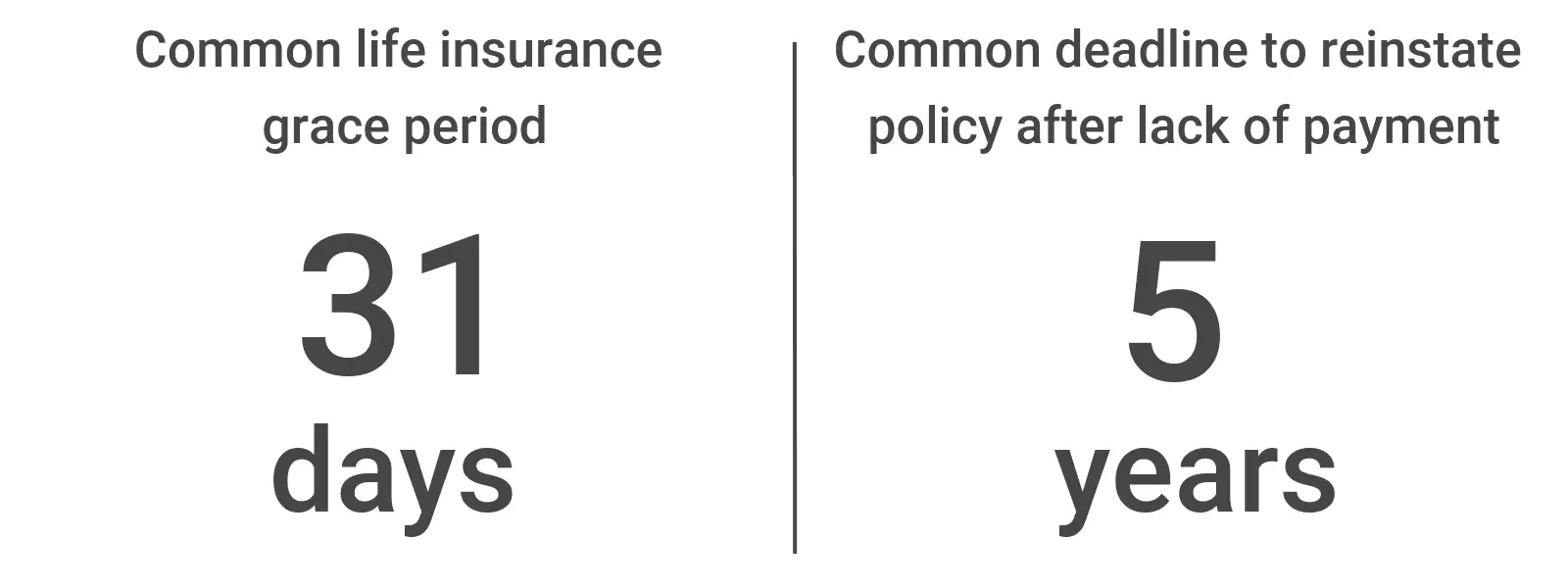
What Kind Of Grace Period Will My Insurance Have
The duration of a grace period depend on a number of factors, the most important of which is the terms of your contract. Some insurance policies don’t have a grace period at all. Grace periods are common for car, health, life, and home insurance, but may be granted with other types of insurance such as business insurance. State law requires a grace period for certain types of insurance, too.
You’ll need to check your specific insurance policy to see what terms it gives for a grace period. Note that paying your premium during the grace period might incur penalties or extra fees.
Also Check: Kroger Employee Discount Card
Health Coverage Tax Credit
The Trade Act of 2002 created a tax credit for certain individuals who become eligible for trade adjustment assistance and for certain retired employees who are receiving pension payments from the Pension Benefit Guaranty Corporation . Eligible individuals can either take a tax credit or get advance payment of 72.5% of premiums paid for qualified health insurance including COBRA. While the HCTC expired on January 1, 2014, it was reinstated to be effective for coverage periods through 2019. For more information, visit, www.irs.gov/HCTC
How Long Will My Health Insurance Cover Me If I Was Fired
Upon firing, it’s up to your employer to determine how long you may continue employer-sponsored health insurance coverage. Ask your company’s human resources representative this question. Many factors determine the answer, including work and severance agreements, how often your employer pays the premium and frequency of health insurer eligibility updates. Lastly, continuation of health insurance is often available to employees upon termination, usually at an additional cost, per COBRA guidelines.
Recommended Reading: Substitute Teacher Health Insurance
How To Prepare To Leave A Job
Before quitting your job, review all of your options for health insurance. Remember that everyones medical and financial situations are different. You might benefit from continuing coverage via COBRA, or it may make more sense to join an individual plan through the marketplace.
Use these tips to make sure youre covered when your employer-sponsored insurance expires:
- Talk with your HR representative before you resign to learn how your employers insurance plan works and when youll lose coverage.
- Consider quitting earlier in the month if your company lets you keep coverage until the last day of the month. This could give you the time you need to get new coveragesuch as from a new employerwithout having to pay for COBRA.
- Gather any documents youll need to enroll in your new health insurance plan. For example, the marketplace offers a convenient checklist to help you apply for a plan.
When Coverage Expires And How To Replace It
You gave your boss a resignation letter. You completed an exit interview with human resources. Your co-workers threw you a going-away party. Youre all set to leave your job and move on to your next adventure.
Thats when it hits you: You have no idea when your employer-sponsored health insurance ends, let alone how to get coverage on your own.
Figuring out health insurance after leaving a job can be frustrating and confusing. But you can make the transition from your old coverage as smooth as possible by being prepared. Read on to learn when your health coverage ends and what options you have once it expires.
Don’t Miss: What Insurance Does Starbucks Offer
What Happens When The Grace Period For Ones Term Life Insurance Ends
If you choose not to renew your term life insurance during the grace period, your term life plan will lapse and the policy will no longer be valid. A lapsed policy means that all your term insurance premiums that were paid so far, in addition to the coverage secured may be lost. Any claims that are raised on a policy that has lapsed are void.
These claims are simply rejected by the insurer. However, if the policyholder were to die during the grace period, his family is eligible to receive the death benefit after deduction of the unpaid premium. Overall, it is recommended that one should never let their term policy lapse to begin with by making timely premium payments.
Life Insurance Policy Grace Period Law Is Not Retroactive California Appellate Court Rules
A California court has ruled that an amendment to the insurance law providing a 60-day grace period before a life insurer may terminate a life insurance policy for nonpayment of premiums that came into effect on January 1, 2013 did not apply to term life insurance policies issued before that date.
You May Like: Does Kroger Offer Health Insurance To Part Time Employees
Loss Of Other Group Health Plan Coverage
If, while you are enrolled for COBRA Continuation Coverage your Spouse or Dependent loses coverage under another group health plan, you may enroll the Spouse or Dependent for coverage for the balance of the period of COBRA Continuation Coverage. The Spouse or Dependent must have been eligible but not enrolled in coverage under the terms of the pre-COBRA Plan and, when enrollment was previously offered under that pre-COBRA healthcare Plan and declined, the Spouse or Dependent must have been covered under another group health plan or had other health insurance coverage.
The loss of coverage must be due to exhaustion of COBRA Continuation Coverage under another plan, termination as a result of loss of eligibility for the coverage, or termination as a result of employer contributions toward the other coverage being terminated. Loss of eligibility does not include a loss due to failure of the individual or participant to pay premiums on a timely basis or termination of coverage for cause. You must enroll the Spouse or Dependent within 31 days after the termination of the other coverage. Adding a Spouse or Dependent Child may cause an increase in the amount you must pay for COBRA Continuation Coverage.
Reducing The Grace Period Would Weaken The Marketplace
Hastily terminating coverage for late payment could end coverage for a large number of marketplace enrollees who simply forgot to pay on time. This would push them out of the insurance marketplace until the following year unless they had a life change qualifying them for a special enrollment period. To the extent that a bigger pool improves risk, this diminishing overall enrollment could negatively impact others marketplace premiums.
If one missed premium payment leads to a loss of coverage, the marketplace risk pool as a whole may suffer from the departure of healthy people and their inability to reenroll. While we dont have data on the characteristics of late-payers or the health status of people whose coverage is discontinued due to nonpayment, it stands to reason that sicker people will make the greatest efforts to maintain their coverage whereas healthier people may believe that they have less to lose by letting insurance lapse. If this is true, we would expect the people who exit the marketplace due to nonpayment to be healthier, on average. And because young adults who also tend to be healthier are 25 percent likelier to pay bills late than older adults, those exiting enrollees may skew younger and healthier as well.
Read Also: How Long Insurance After Quitting
How Much Does Part B Cost
The Social Security Act sets out the Medicare premiums, deductibles, and copays each year.
An individualâs income determines what they will pay for their Medicare Part B monthly premium. For individuals with an income below $88,000, the standard premium is $148.50 in 2021, with an annual deductible of $203.
According to the Centers for Medicare and Medicaid Services, about 7% of Medicare Part B beneficiaries will pay a higher income adjusted premium.
Can I Enroll Again During Open Enrollment If My Old Plan Terminated For Non

Open enrollment has generally allowed people a chance to start over each year with new coverage, regardless of whether the prior years coverage was terminated during the year due to non-payment. But the that were finalized by HHS in 2017 made some changes that allow insurers to recoup past-due premiums when people try to re-enroll during open enrollment.
The new rules are described in more detail here, but essentially, if your coverage is terminated for non-payment of premium and you then enroll in a plan offered by that same insurer within 12 months of your prior plan being terminated, the insurer can require you to pay your past-due premium before effectuating your new policy.
If your coverage was already terminated for non-payment of premiums, the most you would owe in past-due premiums is one month of premiums, as your plan termination date would have been the end of the first month of the grace period. If you werent getting a premium subsidy, you wouldnt have any past-due premiums, because your plan would have been terminated to the last date that you had paid for the coverage .
But if youre still in the grace period when youre re-enrolling , you could owe up to three months of past-due premiums if youre re-enrolling with the same insurer.
Don’t Miss: Insusiance
